Robert and I have the same blood type, A+, and we have known that since we were expecting our daughter in 2015. I knew there may be a chance for us to match but that it would be much more likely for one of his blood relatives.
In August of 2016, I made the call to living donor services to express my interest in being tested. Robert was actually not aware that I had been planning to call until later that day. Knowing that we had the same blood type and that, for medical reasons, a lot of his close relatives could not donate, I figured that I should at least try. I knew that if I didn’t at least attempt, I would always wonder if I would have matched.
A few days following the initial call, I had a 90 minute questionnaire over the phone with the donor transplant coordinator. She asked me questions about my lifestyle as well as my personal and family medical history. She then explained to me what the steps of testing were and what I could expect through the process.
Here in Alberta, the living donor services is completely separate from the recipient services; therefore, very little is actually shared between the organizations. They even tell you that if you have any second thoughts and want to back out, you can do so with no questions. The recipient would not know that you chose not to continue; they would only be told that you weren’t a good match. Not that this mattered to me at all, but it could be quite an intimidating process and the fear of not being able to discreetly back out could be a make or break for those who are considering getting tested.
The thing with donating, is that the main priority is the donor’s health to make sure that they are healthy enough that, by giving a kidney, their health will not be jeopardized if there are unknown risks, diseases or medical conditions.
Depending on where the testing is taking place, they may do the testing prior to finding out if the donor is a match, as they do here in Alberta, Canada. Or they may do the crossmatch testing first like they do in most of the United States. As impatient as I am, I do like doing the health testing based on the fact that some people have certain health conditions that would make it look on the cross match testing as though they are not a match, even when they are. The downfall? Lots of testing and time put in before you even know if you match.
After the questionnaire, they sent me a package of information, brochures and requisitions for multiple tests.
To start with I had to:
- have a bunch of blood taken
- Have an ECG (to check my heart health)
- give a urine sample (urinalysis)
- do a 24 hour urine test where I had to pee in a jug for a full 24 hours (this is the one I disliked the most)
- have a TB (Tuberculosis) Skin test
- do a 3-hour blood glucose test
- have a chest xray
- have an abdominal ultrasound (to see the layout of my abdomen and make sure that I wasn’t born with only one kidney, which is actually more common than you would think)
I (finally) completed the above list of tests on January 12, 2017. This goes to show that these are time consuming for those of us who work full-time and can’t pound it all out in a few weeks.
As I mentioned above, my least favourite test was the 24 hour urine. I was instructed to pick up a urine collection jug from a laboratory, then, on the day of testing, to have my first pee of the day in the toilet and mark the time on the jug as my ‘Start Time’. After that, all of the pee in the next 24 hours had to go into the jug, including the first pee the morning after. Then I had to take the big jug of pee to the lab and have blood drawn to go with it. I had to choose to do it on a day where I was going to be home most of the day because I couldn’t carry the jug with me and I couldn’t leave any pee out.
The first issue that I had was that they only gave me one jug and I am a person who tends to drink lots of fluids and pee a lot. So, needless to say, that jug was filled up before dinner. I did the test on a Sunday, so my lab was not open to get another jug. In a panic, i turned to google and then sent my fiancé to the store to buy a clean container to collect the rest of my urine for the remainder of the 24 hours. Apparently you are not supposed to do that and only the pee that was in the jug could be used for the test.
They also never discussed proper storage for the pee jug. So I kept it on the shelf in my bathroom for easy access. Apparently that was wrong as well and it is supposed to be kept cool (like a fridge or cold garage).
A week or so later, my coordinator contacted me to tell me that the result for the 24 hour urine test was not good (obviously because I wasn’t instructed on how to do it properly from the lab). I was asked to repeat the test where I did it properly; I even kept my pee jug in our fridge (I think it weirded Robert out having a jug of pee beside the milk but whatever). The second result came back with amazing results.
Any test that comes back weird or failed is always redone to confirm and make sure there was not just a problem with the test. This was great because, as much as I did not want to redo anything (especially the 24 hour urine), it took some of the pressure off by knowing that I had another chance if something wasn’t quite right.
My next set of tests was in the big city, a 5 hour drive away on February 22, 2017. I was required to have a PAP test done by my family doctor prior to this date.
This busy day of appointments included:
- Bloodwork for the crossmatch and tissue typing (to see if Robert and I matched FINALLY)
- Urine test
- ECG (another one because the results of my first one never were recorded or sent to the donor coordinator)
- Radioisotope GFR Scan with split function and fluid Loading (they injected radioactive dye into my arm through an IV, then I had to lay under a scanning machine for 45 minutes, then have blood drawn 1 hour after the injection and again 2 hours after that. This test shows the kidneys filtering the radioactive substance from my body and it measures the levels of the substance in my blood 1 and 3 hours after injection to be sure my kidneys were filtering properly).
- Appointment with a transplant social worker (where they do a psychological evaluation, ensure that I was not being paid or pressured/forced to donate, discuss financial factors, etc)
This was a very LONG day but it went quite well overall. And I was back to playing the waiting game.
On March 7 2017, my transplant coordinator called to tell me that the Crossmatch was negative (WHICH IS GOOD!), meaning that our blood didn’t fight. And they were going to be booking me in to meet with a nephrologist (kidney specialist).
I had to go back to the big city for April 6 and 7, 2017 for the next stage of testing.
April 6 was the meeting with the nephrologist. He went over all of the tests that I had done and asked me some questions. He was very impressed with my health but said that I had to redo the 24 hour urine (again!) because of the poor result I got the first time. With the first test being bad and the second result being awesome, he wanted to ensure that the second result was the correct and consistent one.
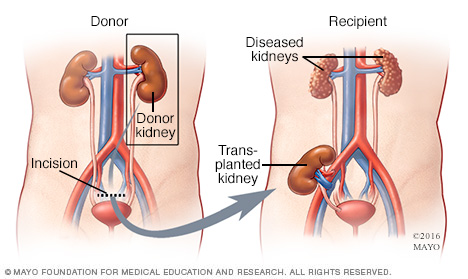
April 7 was my abdominal CT with contrast dye. This CT is a map for the surgeon, so that they can see the layout of my abdomen and where my major vessels are located to assess the risks involved and which side would be better to take from if I did make it to surgery. It also shows them the size of my kidneys and how many viens and arteries are going to each kidney (normal is having 1 vein and 1 artery but some people have 2-3 of each and that can increase risks).

I went home and, a week or so later, I completed the 24 hour hour urine test for the third time.
It took a while to hear anything back but i finally got the call on May 3. My 24 hour urine test got another amazing result and the nephrologist figured that i am a good match and candidate for surgery. He signed me off to go on to the next step: meeting the surgeon on May 8.